Why SHAARPEC?
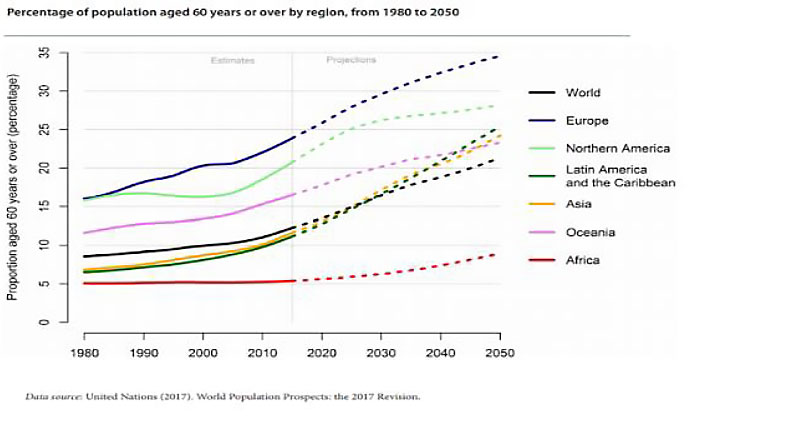
All societies face the challenge of rising healthcare costs, driven by aging populations and an increasing demand for complex diagnostics and treatments.
All societies face the challenge of rising healthcare costs, driven by aging populations and an increasing demand for complex diagnostics and treatments.
Demand for healthcare services continues to rise globally as populations age and individuals live longer with more chronic diseases, which often results in more frequent acute exacerbations requiring acute unscheduled care and advanced diagnostics and treatments. In addition, the continuous development of new diagnostic and treatment options drives demand for these service among the public, who wish to take advantage of these. Global healthcare continues to grow at a faster rate than GDP in many countries. Average healthcare spending among OECD countries is approximately 10% of GDP. The U.S. is the world leader in healthcare spending at nearly twice that amount, i.e. 18%. The growth rates in healthcare spending are not sustainable over the long team. Increasing spending does not necessarily mean higher quality of care.
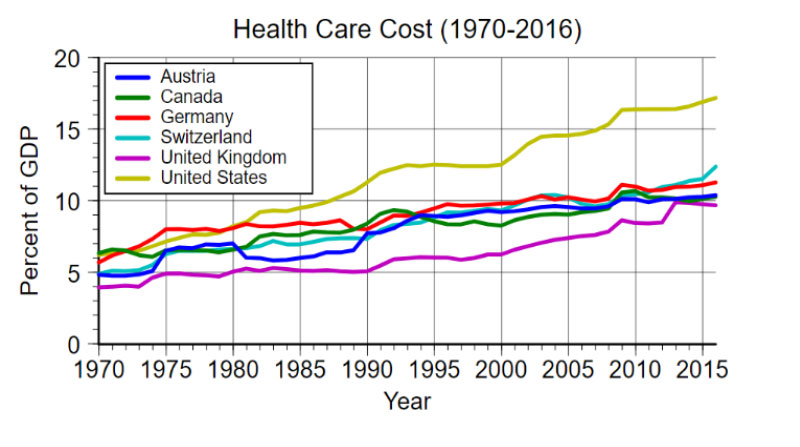
Healthcare cost in relation to GDP 1970–2016. Source: OECD. These growth rates in healthcare spending are not sustainable over the long term.
Healthcare delivery systems tend to be organized by specialty silos and sectors of care delivery built around the providers of care, not the patients who receive care. In addition, the associated data gathering, analysis, quality and performance measurement, budget and financial management also tend to be organized around these silos and not the patient populations served by the system.
In fact, few healthcare systems function as well-integrated systems. Most function as a fragmented group of affiliated silos and sectors that are managed individually with a focus on optimizing their own budget, resources and production.
When we try to understand how care is delivered by healthcare organizations, it is relatively easy to understand and analyze the care delivered within each silo, but more difficult to understand how care is utilized by patient populations across the system of silos.
The organization of data tends to follow the organization of the operations, which – from the perspective of horizontal patient trajectories across the system – is fragmented.
Financial management in healthcare tends to focus on managing silo budgets rather than understanding how they all roll up into a system level budget and managing from that perspective. This, in turns, leads to suboptimization at a system level, i.e. the silos are optimized at the expense of the whole system.
To address the ever-increasing complexity in healthcare we must optimize care delivery for the patient through the whole system, across organizational silos.
Financial accounting in most healthcare systems does not provide robust understanding of actual cost of care delivery at the patient encounter level across the spectrum of care delivery. Costs in healthcare are often reported as average cost per patient encounter, rather than the actual cost of each patient encounter. This limits our ability to analyze the variability in costs, which is necessary in order to identify opportunities for improvement. Furthermore, different organizations might calculate the cost of the same encounter differently, making cross-organization comparisons difficult. Allocation of fixed cost in healthcare systems rarely reflects unused capacity, which precludes meaningful cost trend analyses over time.
Enormous and ever-growing amounts of data are generated in healthcare, however the degree to which we analyze that data and derive actionable insights is limited. As more healthcare systems move to adopt electronic health records (EHRs), the rate of production of new electronic healthcare data is increasing. The advent of wearable personal monitoring devices, low-cost genomic sequencing and other technology trends is further increasing the rate of growth in production of healthcare data. Healthcare organizations tend to focus on gathering more and different types of data, but less on how to analyze existing data to produce the information and insights needed to make better decisions about healthcare system improvement and patient care. Without understanding the effect of an intervention on the patient pathway, healthcare systems run the risk of misallocation of resources, as well as implementing costly interventions with low returns.
The analysis capability required is often beyond the core competencies of healthcare organizations.
Contact us